Rigid Flat Feet In Adults
Overview
Adult flatfoot may be due to multiple problems including a dysfunctional posterior tibial tendon (PTT), hypermobility and ligamentous laxity, or possibly a coalition that becomes symptomatic. For a vast majority of patients, posterior tibial tendon dysfunction (PTTD) is the cause of symptomatic flatfoot and is the main trigger of surgical reconstruction in flatfoot. The common presenting scenario for adult flatfoot is a case of unilateral flatfoot with pain. Patients will often confirm they ?always had flat feet? but have noticed increased pain and additional collapse in the past few months to years. They may also note increased swelling and a possible concern over one foot increasing in shoe size. After a comprehensive dermatologic, neurologic and vascular assessment, one should direct his or her attention to the musculoskeletal portion of the exam. It is key to examine the foot and leg as a whole in order to determine the proper procedure and consider each phase of the corrective surgery. 
Causes
As the name suggests, adult-acquired flatfoot occurs once musculoskeletal maturity is reached, and it can present for a number of reasons, though one stands out among the others. While fractures, dislocations, tendon lacerations, and other such traumatic events do contribute to adult-acquired flatfoot as a significant lower extremity disorder, as mentioned above, damage to the posterior tibial tendon is most often at the heart of adult-acquired flatfoot. One study further elaborates on the matter by concluding that ?60% of patients [presenting with posterior tibial tendon damage and adult-acquired flatfoot] were obese or had diabetes mellitus, hypertension, previous surgery or trauma to the medial foot, or treatment with steroids?.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex.
Non surgical Treatment
PTTD is a progressive condition. Early treatment is needed to prevent relentless progression to a more advanced disease which can lead to more problems for that affected foot. In general, the treatments include rest. Reducing or even stopping activities that worsen the pain is the initial step. Switching to low-impact exercise such as cycling, elliptical trainers, or swimming is helpful. These activities do not put a large impact load on the foot. Ice. Apply cold packs on the most painful area of the posterior tibial tendon frequently to keep down the swelling. Placing ice over the tendon immediately after completing an exercise helps to decrease the inflammation around the tendon. Nonsteroidal Anti-inflammatory Medication (NSAIDS). Drugs, such as arcoxia, voltaren and celebrex help to reduce pain and inflammation. Taking such medications prior to an exercise activity helps to limit inflammation around the tendon. However, long term use of these drugs can be harmful to you with side effects including peptic ulcer disease and renal impairment or failure. Casting. A short leg cast or walking boot may be used for 6 to 8 weeks in the acutely painful foot. This allows the tendon to rest and the swelling to go down. However, a cast causes the other muscles of the leg to atrophy (decrease in strength) and thus is only used if no other conservative treatment works. Most people can be helped with orthotics and braces. An orthotic is a shoe insert. It is the most common non-surgical treatment for a flatfoot and it is very safe to use. A custom orthotic is required in patients who have moderate to severe changes in the shape of the foot. Physiotherapy helps to strengthen the injured tendon and it can help patients with mild to moderate disease of the posterior tibial tendon. 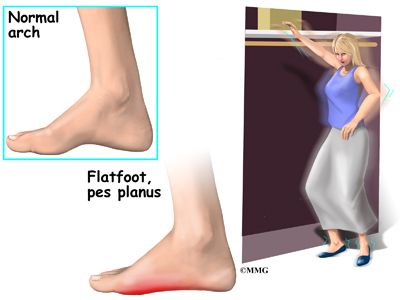
Surgical Treatment
For patients with a more severe deformity, or significant symptoms that do not respond to conservative treatment, surgery may be necessary. There are several procedures available depending on the nature of your condition. Ligament and muscle lengthening, removal of inflamed tendon lining, transferring of a nearby tendon to re-establish an arch, and bone realignment and fusion are examples of surgical options to help with a painful flatfoot condition. Surgery can be avoided when symptoms are addressed early. If you are feeling ankle pain or notice any warmth, redness or swelling in your foot, contact us immediately. We can create a tailored treatment plan to resolve your symptoms and prevent future problems.