Sharp Pain In Foot Arch And Ankle
High arch (cavus foot) is a condition in which the arch on the bottom of the foot that runs from the toes to the heel is raised more than normal. Because of this high arch, excessive weight falls on the ball and heel of the foot when walking or standing causing pain and instability. Children with neurological disorders or other conditions such as cerebral palsy, spina bifida, poliomyelitis, muscular dystrophy are more likely to develop cavus foot. It may sometimes occur as an inherited abnormality.

Causes
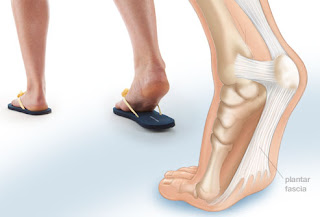
The plantar fascia is a thick, fibrous band which runs along the sole of the feet. It helps to support the foot arches and transmits forces through the foot as you move. Plantar fasciitis is one of the most common causes of foot arch pain. The most common problem to develop here is plantar fasciitis. If there is too much strain on the plantar fascia (e.g. from long periods on your feet, suddenly increasing activity levels or your foot position is altered), the plantar fascia becomes inflamed and swollen. It is often accompanied by a bone spur, excess growth of the bone which develops due to repeated tension on the area where the plantar fascia attaches to the bone. Plantar fasciitis is one of the most common causes of foot arch pain. It is usually painful after activity or prolonged rest e.g. first thing in the morning. A less common problem with the plantar fascia which casues foot arch pain is plantar fibromatosis. This is when a small nodular growth develops on the plantar fascia, usually in the middle of the foot arch. It often causes pain when walking due to pressure through the lump.
Symptoms
The muscle imbalance around the foot and ankle gives rise to a typical pattern of deformity in addition to the high arch (known as cavus). The bone under the big toe (called the first metatarsal) can become very prominent and the toes can curl or clench like a fist (called claw toes). Excessive amount of weight may be placed on the ball and heel of the foot, which can lead to the ankle weakening and giving way (this is referred to as ankle instability) and soreness. Calluses and sometimes stress fractures may occur where the foot is exposed to extra friction or pressure, such as on the outer (or lateral) border of the foot.
Diagnosis
To come to a correct diagnosis, your podiatrist will examine your foot by using his or her fingers to look for a lump or stone bruise in the ball of your foot. He or she will examine your foot to look for deformities such as high or low arches, or to see if you have hammertoes. He or she may use x-rays, MRIs (magnetic resource imaging), and CT scans to rule out fractures and damage to ligaments, tendons, and other surrounding tissues. Your doctor will also inquire about your daily activities, symptoms, medical history, and family history. If you spend a lot of time running or jumping, you may be at a higher risk for pain in the bottom of your foot. These diagnostic tests will help your doctor come to a proper diagnosis and create an appropriate treatment plan.
Non Surgical Treatment
If you have arch pain, you need proper arch support. You can get arch support by purchasing custom shoe inserts that are made to support your feet. If you have flat feet or high arches, you can certainly benefit from arch support inserts. Take a look at your wet footprint; if you notice that your footprint is completely filled in, then you have flat feet. On the other hand, if there is a large crescent shape missing from your footprint, then you have high arches. Both of these conditions require proper support from a shoe insert. Foot Solutions You can also take care of your feet by avoiding high heels and flip-flops. If you must wear high heels, choose a heel that is two inches or less, and try to wear them only for short periods of time. Flip-flops provide very little support, so wear them only if you won?t be doing very much walking.

Surgical Treatment
Foot surgery is difficult, especially when large amounts of deformity correction are needed. The ability to bring the foot into a new position may not be lasting, even if everything looks perfect in the operating room. The goal is to provide improved position and function of the foot and ankle. In some patients with very severe deformity, the goal is a foot that functions well in a brace. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Particular complications associated with cavus foot surgery include incomplete correction of deformity, return of deformity and incomplete fusion.
Prevention
Drink plenty of water before, during and after your workout. Dehydration is a common cause of muscle cramps, according to MayoClinic.com. If your workouts are long and strenuous, drink a carbohydrate-based electrolyte beverage too. Warm up the muscles of your feet before you work out. A simple exercise is to write the letters of the alphabet with your toes. Perform the warm up with bare feet and exaggerate the movements to challenge your muscles. Wear properly fitted shoes. Visit a sporting goods store and get your feet and arches measured. Ask for help selecting a pair of shoes to fit your workout. For instance, if you play soccer, you need cleats, not running shoes. Take a break. Cramps can be your body's way of telling you you're exercising too much, according to MayoClinic.com. Rest for a few days, then resume exercise and see if you can complete a workout without arch cramps. Stretch. At the end of your workout, perform a few stretching exercises to keep your muscles from tightening and cramping. Sit down, lean over and grasp your toes. Pull the toes toward your body until you feel tension in the arch of your foot. Hold the stretch for 20 to 30 seconds, then repeat on the opposite side. Another easy way to stretch your arch is to put a towel on the floor, curl your toes around it and pull it toward your body.
Stretching Exercises
Achilles stretch. Stand with the ball of one foot on a stair. Reach for the step below with your heel until you feel a stretch in the arch of your foot. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Balance and reach exercises. Stand next to a chair with your injured leg farther from the chair. The chair will provide support if you need it. Stand on the foot of your injured leg and bend your knee slightly. Try to raise the arch of this foot while keeping your big toe on the floor. Keep your foot in this position. With the hand that is farther away from the chair, reach forward in front of you by bending at the waist. Avoid bending your knee any more as you do this. Repeat this 15 times. To make the exercise more challenging, reach farther in front of you. Do 2 sets of 15. While keeping your arch raised, reach the hand that is farther away from the chair across your body toward the chair. The farther you reach, the more challenging the exercise. Do 2 sets of 15. Towel pickup. With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel. Resisted ankle plantar flexion. Sit with your injured leg stretched out in front of you. Loop the tubing around the ball of your foot. Hold the ends of the tubing with both hands. Gently press the ball of your foot down and point your toes, stretching the tubing. Return to the starting position. Do 2 sets of 15. Resisted ankle dorsiflexion. Tie a knot in one end of the elastic tubing and shut the knot in a door. Tie a loop in the other end of the tubing and put the foot on your injured side through the loop so that the tubing goes around the top of the foot. Sit facing the door with your injured leg straight out in front of you. Move away from the door until there is tension in the tubing. Keeping your leg straight, pull the top of your foot toward your body, stretching the tubing. Slowly return to the starting position. Do 2 sets of 15. Heel raise. Stand behind a chair or counter with both feet flat on the floor. Using the chair or counter as a support, rise up onto your toes and hold for 5 seconds. Then slowly lower yourself down without holding onto the support. (It's OK to keep holding onto the support if you need to.) When this exercise becomes less painful, try doing this exercise while you are standing on the injured leg only. Repeat 15 times. Do 2 sets of 15. Rest 30 seconds between sets.
The Treatment And Cause
Overview
There are some things that gain value as they age. Antique dealers are always on the lookout for pieces that have a certain ?wear and tear? look that will bring a high price tag. Our feet on the other hand, don?t always fair as well when they have experienced a lot of wear and tear. Cumulative stress and impact can cause your foot structure to weaken and become prone to injury, especially when you have a flat foot. This is the case with a condition called posterior tibial tendon dysfunction. 
Causes
Flat footedness, most people who develop the condition already have flat feet. With overuse or continuous loading, a change occurs where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Inadequate support from footwear may occasionally be a contributing factor. Trauma or injury, occasionally this condition may be due to fracture, sprain or direct blow to the tendon. Age, the risk of developing Posterior Tibial Tendon Dysfunction increases with age and research has suggested that middle aged women are more commonly affected. Other possible contributing factors - being overweight and inflammatory arthritis.
Symptoms
Initially, flatfoot deformity may not present with any symptoms. However, overtime as the tendon continues to function in an abnormal position, people with fallen arches will begin to have throbbing or sharp pain along the inside of the arch. Once the tendon and soft tissue around it elongates, there is no strengthening exercises or mechanism to shorten the tendon back to a normal position. Flatfoot can also occur in one or both feet. If the arch starts to slowly collapse in one foot and not the other, posterior tibial dysfunction (PTTD) is the most likely cause. People with flatfoot may only have pain with certain activities such as running or exercise in the early phase of PTTD. Pain may start from the arch and continue towards the inside part of the foot and ankle where the tendon courses from the leg. Redness, swelling and increased warmth may also occur. Later signs of PTTD include pain on the outside of the foot from the arch collapsing and impinging other joints. Arthritic symptoms such as painful, swollen joints in the foot and ankle may occur later as well due to the increased stress on the joints from working in an abnormal position for a long period of time.
Diagnosis
Your podiatrist is very familiar with tendons that have just about had enough, and will likely be able to diagnose this condition by performing a physical exam of your foot. He or she will probably examine the area visually and by feel, will inquire about your medical history (including past pain or injuries), and may also observe your feet as you walk. You may also be asked to attempt standing on your toes. This may be done by having you lift your ?good? foot (the one without the complaining tendon) off the ground, standing only on your problem foot. (You may be instructed to place your hands against the wall to help with balance.) Then, your podiatrist will ask you to try to go up on your toes on the bad foot. If you have difficulty doing so, it may indicate a problem with your posterior tibial tendon. Some imaging technology may be used to diagnose this condition, although it?s more likely the doctor will rely primarily on a physical exam. However, he or she may order scans such as an MRI or CT scan to look at your foot?s interior, and X-rays might also be helpful in a diagnosis.
Non surgical Treatment
A patient who has acute tenosynovitis has pain and swelling along the medial aspect of the ankle. The patient is able to perform a single-limb heel-rise test but has pain when doing so. Inversion of the foot against resistance is painful but still strong. The patient should be managed with rest, the administration of appropriate anti-inflammatory medication, and immobilization. The injection of corticosteroids is not recommended. Immobilization with either a rigid below-the-knee cast or a removable cast or boot may be used to prevent overuse and subsequent rupture of the tendon. A removable stirrup-brace is not initially sufficient as it does not limit motion in the sagittal plane, a component of the pathological process. The patient should be permitted to walk while wearing the cast or boot during the six to eight-week period of immobilization. At the end of that time, a decision must be made regarding the need for additional treatment. If there has been marked improvement, the patient may begin wearing a stiff-soled shoe with a medial heel-and-sole wedge to invert the hindfoot. If there has been only mild or moderate improvement, a longer period in the cast or boot may be tried. 
Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.
Insertional Achilles Tendonitis Boot
 This nagging injury can be long-lasting if not treated - and if your running form needs some work. The name Achilles is said to be a combination of two Greek words that together mean ?grief of the people.? The injury that bears that hero?s name, in honor of his only weakness, certainly aggrieves many runners, with Achilles tendinitis accounting for around 10 percent of running injuries. Technically, Achilles tendinitis is acute inflammation of the tendon that runs along the back of the ankle. Pain in that area for longer than a couple weeks is not really tendinitis anymore. Athletes, however, tend to characterize any pain along the tendon above the back of the heel as Achilles tendinitis. Achilles tendinitis can be confused with other injuries, such as heel problems, but the hallmark sign is if you?re pinching the Achilles and it?s really sore.
This nagging injury can be long-lasting if not treated - and if your running form needs some work. The name Achilles is said to be a combination of two Greek words that together mean ?grief of the people.? The injury that bears that hero?s name, in honor of his only weakness, certainly aggrieves many runners, with Achilles tendinitis accounting for around 10 percent of running injuries. Technically, Achilles tendinitis is acute inflammation of the tendon that runs along the back of the ankle. Pain in that area for longer than a couple weeks is not really tendinitis anymore. Athletes, however, tend to characterize any pain along the tendon above the back of the heel as Achilles tendinitis. Achilles tendinitis can be confused with other injuries, such as heel problems, but the hallmark sign is if you?re pinching the Achilles and it?s really sore.
Causes
Over-pronation, injury and overstresses of the tendon are some of the most common causes. Risk factors include tight heel cords, poor foot alignment, and recent changes in activities or shoes. During a normal gait cycle, the upper and lower leg rotate in unison (i.e. internally during pronation and externally during supination). However, when a person over-pronates, the lower leg is locked into the foot and therefore continues to rotate internally past the end of the contact phase while the femur begins to rotate externally at the beginning of midstance. The Gastrocnemius muscle is attached to the upper leg and rotates externally while the Soleus muscle is attached to the lower leg and rotates internally during pronation. The resulting counter rotation of the upper and lower leg causes a shearing force to occur in the Achilles tendon. This counter rotation twists the tendon at its weakest area, namely the Achilles tendon itself, and causes the inflammation. Since the tendon is avascular, once inflammation sets in, it tends to be chronic.
Symptoms
Symptoms of acute achilles tendonitis will be a gradual onset of achilles pain at the back of the ankle, just above the heel bone. This may develop over a period of days. The achilles tendon may be painful and stiff at the start of exercise and first thing in the morning. As the tendon warms up the pain will go often for it to return later in the day or towards the end of a prolonged training session. The tendon will be very tender on palpation or pressing in on the achilles tendon or squeezing it from the sides. Chronic achilles tendonitis may follow on from acute achilles tendonitis if it goes untreated or is not allowed sufficient rest. Chronic achilles tendonitis is a difficult condition to treat, particularly in older athletes who appear to suffer more often.
Diagnosis
There is enlargement and warmth of the tendon 1 to 4 inches above its heel insertion. Pain and sometimes a scratching feeling may be created by gently squeezing the tendon between the thumb and forefinger during ankle motion. There may be weakness in push-off strength with walking. Magnetic resonance imaging (MRI) can define the extent of degeneration, the degree to which the tendon sheath is involved and the presence of other problems in this area, but the diagnosis is mostly clinical.
Nonsurgical Treatment
There is insufficient evidence from randomised controlled trials to determine which method of treatment is the most appropriate for the treatment of acute or chronic Achilles tendonitis. The patient should abstain from aggravating activities, but with a minimum of rest in order to preserve overall fitness. Possible treatments are non-steroidal anti-inflammatory drugs (NSAIDs), ice, rest, increased warm-up/stretching exercises, physiotherapy and heel lifts (orthotic devices - used on both sides to prevent a gait imbalance). Other treatments evaluated in a Cochrane review were heparin, steroid injections, glycosaminoglycan sulfate, Actovegin?, and topical laser treatment. There was no clear evidence of benefit from these. Casting is an option for resistant Achilles tendonitis. Drugs - analgesics and NSAIDs. Surgery is sometimes used for resistant Achilles tendonitis, but usually as a last resort. Other recently reported treatments include continuing sporting activity in conjunction with rehabilitation, low-energy shock wave therapy[4] and topical glyceryl trinitrate .

Surgical Treatment
Surgery is considered the last resort and is often performed by an orthopedic surgeon. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon. Rehabilitation, including stretching and strength exercises, is started soon after the surgery. In most cases, normal activities can be resumed after about 10 weeks. Return to competitive sport for some people may be delayed for about three to six months.
Prevention
Stretching of the gastrocnemius (keep knee straight) and soleus (keep knee bent) muscles. Hold each stretch for 30 seconds, relax slowly. Repeat stretches 2 - 3 times per day. Remember to stretch well before running strengthening of foot and calf muscles (eg, heel raises) correct shoes, specifically motion-control shoes and orthotics to correct overpronation. Gradual progression of training programme. Avoid excessive hill training. Incorporate rest into training programme.
Pes Planus Explained
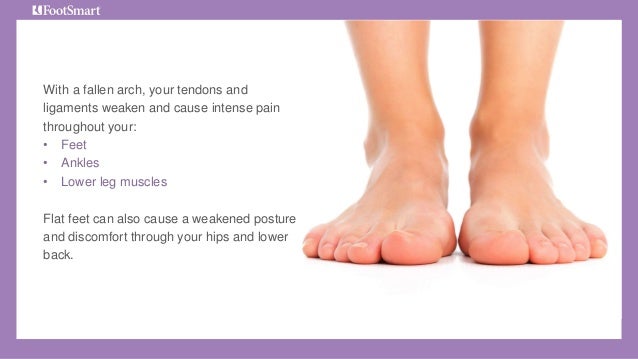
If you take a close look an adult foot (from the inside) you will notice an inward/upward curve at the center. This curve is known as an arch, and it?s formed by tendons in the foot and lower leg attached at the heel and foot bones. When these tendons pull and attach normally, the foot forms a normal arch. When the tendons don?t pull together properly, they don?t form any arch. This results in flat feet popularly known as fallen arches.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Arches can be seen as ?rolling downward? or collapsing when walking. Pain may present in lower back, hips or knees. Pain may be present on the bottom of the heels, within the arch, within the ankles or even the forefoot. Swelling can occur. Pain may occur in the anterior leg muscles.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
Non Surgical Treatment
The typical treatment for pain from fallen arches is an arch insert. While many people experience dramatic pain relief from this, others continue to suffer from chronic achy feet despite the arch support. The problem with this approach is that it does not do anything to strengthen the weak ligaments that may be at the root of the problem and, thus, does not alleviate the chronic pain that people with this condition experience. Another standard practice of modern medicine is to use steroids or to prescribe anti-inflammatory medications. However, in the long run, these treatments do more damage than good. Cortisone shots and anti-inflammatory drugs have been shown to produce short-term pain benefit, but both result in long-term loss of function and even more chronic pain by actually inhibiting the healing process of soft tissues and accelerating cartilage degeneration. Plus, long-term use of these drugs can lead to other sources of chronic pain, allergies and leaky gut syndrome.
Surgical Treatment

Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
Prevention
Flat feet or Fallen Arches cannot be prevented due to congenital of nature or from underlying disease process; however, painful symptoms and future pathology from Flat Feet or Fallen Arches may be prevented by the following. Continue to wear your orthotics for work and exercise to provide stability and maintain function of your feet. Footwear. Continue to wear supportive shoes to maximise the function of your orthotic and prevent excessive movement of the joints in your feet.
Everything You Need To Find Out Regarding Pain In The Arch
Flat feet are a common condition. In infants and toddlers, the longitudinal arch is not developed and flat feet are normal. Most feet are flexible and an arch appears when the person stands on his or her toes. The arch develops in childhood, and by adulthood most people have developed normal arches. Most flat feet usually do not cause pain or other problems. Flat feet may be associated with pronation, a leaning inward of the ankle bones toward the center line. Shoes of children who pronate, when placed side by side, will lean toward each other (after they have been worn long enough for the foot position to remodel their shape). Foot pain, ankle pain or lower leg pain, especially in children, may be a result of flat feet and should be evaluated.

Causes
There are several reasons why arch pain develops. Sometimes it?s due to a condition known as plantar fasciitis, in which the plantar fascia (the band of tissue that runs along the bottom of your foot from your heel to your toes) becomes inflamed after excessive stress. Heel pain results from this inflammation. Sometimes the pain is due to extensive time spent on your feet. Many people feel pain on the arch of their feet after a long workday, while others overuse their feet exercising or playing sports. A foot deformity, such as hammertoe or clubfoot, can also cause this pain. Medical conditions such as diabetes or obesity can put additional stress on your feet, thereby causing arch pain. Your footwear is also important. Shoes should support all parts of your foot, especially the bottom. This is very important if you spend excessive time on your feet, if your obese, if your pregnant, or if you engage in sport-related activities. Injuries to any of the twenty-six bones, thirty-three joints and over 100 muscles, tendons and ligaments in the feet can also cause arch pain. Because the foot is such a complex structure, it?s important to see a podiatrist at the first sign of symptoms.
Symptoms
People suffering from pain in the arch sometimes complain of burning or soreness on the foot sole, which is worse in the morning and after physical activity. There may also be some tenderness when pressure is applied to the sole of the foot or heel. In addition to this, patients tend to complain of more pain when they stand on tiptoe.
Diagnosis
Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
In mild cases of flatfoot the first line of treatment is often custom orthotics. In patients with a flexible deformity, supporting the arch with a custom arch support will take the strain off the joints and muscles, bringing the heel into a corrected position. Wider shoe gear may be prescribed to accommodate foot pain and motion and stretching exercises to decrease stiffness and stress on the foot. In cases of severe collapse, especially if the patient is not a good surgical candidate or has a mild tear, a brace may be made to accommodate the foot and ankle, thus supporting the arch and ankle.

Surgical Treatment
If pain or foot damage is severe, your doctor may recommend surgery. Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
Prevention
Arch pain occurs when the plantar fascia becomes worn down due to constant strain or excessive exercising. This may be caused by increasing your running or hiking mileage too fast, wearing inadequate footwear, lack of stretching, running on steep hills, standing on your feet for too long and abnormal anatomy such as flat foot. Stretching is an important exercise that should not be overlooked because the tightness or lack of tightness of the joints in the foot can also cause pain in the arch.
Stretching Exercises
Easy Beginner Version. Start with your bare foot on a flat surface, toes spread out. Place a penny under the ball of your foot and the end of a pen under the middle of your arch (sticking out from the inside of your foot). Activate your arch by flexing your arch muscle. You should feel the muscles on the ball of your foot pushing down on the penny, but your arch shouldn't be pushing down on the pen. These tools help you (1) avoid rolling your foot and (2) avoid pressing down with your toes (as an extra tip, you can slide a business card under your toes before doing the exercise-when you activate your arch, you should be able to slide the business card out easily with your fingers). Do your best to keep your toes relaxed. Advanced Version. Once you're ready to move on, you can try this advanced version. It builds on the above exercise to incorporate full body twisting and balance, helping you to maintain proper arches while you move. Using the same ideas from above, stand on a flat surface in your bare feet with a penny under the ball of your foot and the end of a pen under your arch. This time, stand with your back a few inches away form a wall or a door. Lift your other leg (the one without the penny or pen) and stand on one foot. Use the wall for balance, if necessary. Lift one arm and stretch it across your body until you touch the wall or door on the opposite side, maintaining a straight back. Keep your foot straight and your arch on the penny but above the pen. Your arch will want to follow the movement and roll off, but you will need to activate it to stay stable during the movement. Lift your other arm and stretch it across the opposite side of your body, still keeping your arch in place.
Adult Aquired FlatFoot Causes
Over 60 Million Americans have problems with Adult Acquired Flatfoot (AAF), normally called Posterior Tibial Tendon Dysfunction or even PTTD. This particular situation usually occurs in adults coming from 40-65 years of age, also it usually just occurs in one foot, not both. The Particular Posterior Tibial (PT) Tendon courses over the inside a part of the particular ankle along with underneath the particular arch in the foot. That is the main supporting construction for that arch. over time, the tendon becomes diseased, via overuse, and also starts to lose it's strength. As any result, the arch starts to collapse, putting further strain about the PT Tendon, leading to further decline in tendon strength, that brings about further collapse in the arch. This is described like a progressive deformity since it will generally get worse more than time.
Causes
There tend to be multiple elements contributing towards the progression of this problem. Damage to the nerves, ligaments, and/or tendons of the foot could cause subluxation (partial dislocation) in the subtalar or talonavicular joints. Bone fracture can become a feasible cause. The Particular resulting joint deformity through any one of these issues can result in adult-acquired flatfoot deformity. Dysfunction in the posterior tibial tendon features always been linked together with adult-acquired flatfoot deformity (AAFD). the loss involving active and also passive pull in the tendon alters the actual regular biomechanics with the foot and ankle. Your reasons for this can always be many as well as varied as well. Diabetes, substantial blood pressure, as well as prolonged use regarding steroids are usually a variety of the much more typical brings about associated with adult-acquired flatfoot deformity (AAFD) brought in by impairment of the posterior tibialis tendon. Overstretching or rupture in the tendon leads to tendon along with muscle imbalance inside the foot resulting in adult-acquired flatfoot deformity (AAFD). Rheumatoid arthritis will be among the greater common causes. Regarding 1 / two of just about all adults using this type involving arthritis will develop adult flatfoot deformity more than time. Inside such cases, the situation is actually gradual as well as progressive. obesity may be linked with this condition. Loss of blood supply for any reason within the region with the posterior tibialis tendon is an additional factor. Additional achievable causes include bone fracture or even dislocation, the torn as well as stretched tendon, or a neurologic issue causing weakness.
Symptoms
The the indicators of PTTD might include pain, swelling, a flattening in the arch, and also inward rolling of the ankle. Because the condition progresses, the symptoms will change. Pertaining To example, later, because the arch starts to flatten, there could still be pain on the inside of the foot as well as ankle. However only in that point, the actual foot and toes commence to turn outward and in addition the ankle rolls inward. While PTTD gets to become more advanced, the actual arch flattens even more as well as the pain frequently shifts for the outside involving the foot, under your ankle. the tendon offers deteriorated considerably along with arthritis frequently develops within the foot. Throughout a lot more severe cases, arthritis might also develop inside the ankle. Symptoms, which may occur in some persons using flexible flatfoot, include. Pain within the heel, arch, ankle, as well as over the not in the foot. ?Turned-in? ankle. Pain related using a shin splint. General weakness / fatigue within the foot or perhaps leg.
Diagnosis
The diagnosis involving tibialis posterior dysfunction is actually essentially clinical. However, plain radiographs in the foot and ankle are generally ideal for assessing the actual level of deformity and to confirm the actual presence or absence of degenerative changes inside the subtalar as well as ankle articulations. the radiographs are also useful to exclude additional causes of an acquired flatfoot deformity. Your many helpful radiographs are generally bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) take a glance at the actual ankle. Almost All radiographs needs for you to be completed with the affected person standing. in many instances we see zero role for magnetic resonance imaging or even ultrasonography, as the diagnosis can become made clinically.
Non surgical Treatment
Flatfoot deformity may be treatable conservatively or even using surgical intervention depending about the severity of the condition. Whenever folks discover their arches flattening, these people ought to right away steer clear of non-supportive shoes for example flip-flops, sandals as well as thin-soled tennis shoes. Theses shoes will simply worsen your flatfoot deformity and also exacerbate arch pain. Next, custom orthotics tend to be important with regard to individuals with collapsed arches. Over-the-counter insoles just supply cushion and also padding towards the arch, whereas custom orthotics are fabricated for you to particularly in shape the particular patient?s foot and offer support inside the arch the area exactly where the posterior tibial tendon is actually unable to anymore. Use associated with custom orthotics in the early phases associated with flatfoot or even PTTD could stop worsening involving signs as well as stop further attenuation or perhaps injury to the posterior tibial tendon. Throughout a lot more severe cases of flatfoot deformity an ankle foot orthosis (AFO) such like a Ritchie brace is needed. This kind of brace provides more support to the arch and also hindfoot as opposed to an orthotic but can end up being bulky inside typical shoegear. Extra treatment in addition to use associated with custom orthotics can be use regarding non-steroidal anti-inflammatories (NSAIDS) such as Advil, Motrin, or Ibuprofen that could lower inflammation for the posterior tibial tendon. When pain can be severe, the individual may need to be placed inside a under the actual knee air walker boot for a quantity of weeks which will enable the tendon to rest and heal, particularly if a posterior tibial tendon tear is noted upon MRI.

Surgical Treatment
In cases exactly where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The Particular objective regarding surgery along with non-surgical remedy is usually to remove pain, quit progression with the deformity along with boost mobility of the patient. Opinions vary as towards the very best surgical treatment pertaining to adult acquired flatfoot. Processes generally used to appropriate the actual issue consist of tendon debridement, tendon transfers, osteotomies (cutting and also repositioning of bone) and joint fusions. (See surgical correction of adult acquired flatfoot). Patients together with adult acquired flatfoot tend to be suggested to talk about thoroughly the benefits vs. risks of surgical options. The Majority Of processes have long-term recovery mandating that the right procedure be applied to supply the greatest long-term benefit. Nearly All flatfoot surgical procedures call for six for you to twelve weeks involving cast immobilization. Joint fusion procedures require eight weeks associated with non-weightbearing around the managed foot - meaning anyone is likely to be in crutches for two months. The Particular bottom line is, Make sure just about all of one's non-surgical choices have been covered just before contemplating surgery. Your Current main objectives together with just about any therapy will end up being to get rid of pain and boost mobility. Throughout many cases, using the correctly designed foot orthosis or even ankle brace, these goals may be performed with out surgical intervention.
What Might Cause Pain In The Arches ?
Flat feet, also known as ?fallen arches? are often viewed as problematic simply because they look abnormal, the main arch of the foot, the medial longitudinal arch, has collapsed. Though flat feet are by no means normal, they are often the result of some other underlying condition or weakness rather than a problem with the actual arch itself that has collapsed. Conventional treatment involving foot support either via supportive footwear, orthotics, or some other bracing system is usually more disadvantageous than beneficial and surgery is rarely the answer.
Causes
Sprains, strains, bruises, and fractures may be the result of a single stress or a combination of stresses to the foot. A blunt-force injury such as someone stepping on your foot may result not only in a bruise (contusion), but also in damage to the primary and secondary structures of the foot. Many of the muscles of the lower leg and foot attach on or near the arch. Injured or tight muscles may lead to incorrect biomechanics and in turn cause arch pain. Injury to the bones of the foot can be caused by a single blow or twist to the arch or also by repetitive trauma, which can result in a stress fracture. A sprain of the arch occurs when the ligaments which hold the bones together are overstretched and the fibers tear. The muscles of the foot may be strained by overstretching, overuse, overloading, bruising, or being cut by stepping on a sharp object. Arthritis of the arch joints may also occur if the foot is subjected to repetitive movements that stress the arch.
Symptoms
Typically, the sufferer of plantar fasciitis experiences pain upon rising after sleep, particularly the first step out of bed. Such pain is tightly localized at the bony landmark on the anterior medial tubercle of the calcaneus. In some cases, pain may prevent the athlete from walking in a normal heel-toe gait, causing an irregular walk as means of compensation. Less common areas of pain include the forefoot, Achilles tendon, or subtalar joint. After a brief period of walking, the pain usually subsides, but returns again either with vigorous activity or prolonged standing or walking. On the field, an altered gait or abnormal stride pattern, along with pain during running or jumping activities are tell-tale signs of plantar fasciitis and should be given prompt attention. Further indications of the injury include poor dorsiflexion (lifting the forefoot off the ground) due to a shortened gastroc complex, (muscles of the calf). Crouching in a full squat position with the sole of the foot flat on the ground can be used as a test, as pain will preclude it for the athlete suffering from plantar fasciitis, causing an elevation of the heel due to tension in the gastroc complex.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch. An area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle.
Non Surgical Treatment
In addition to relieving the pain by providing better metatarsal support for your feet, many doctors advise stretching and strengthening the muscles that surround the damaged or weakened tendons. This advice can prove especially effective in preventing the possible side effects of fallen arches, including: inflammation and discomfort in the ligaments of the sole, Achilles tendonitis, shin splints, calluses, and bunions. Like plantar fasciitis, left untreated, fallen arches can cause a domino effect that impacts your legs, hips, and back.

Surgical Treatment
If pain or foot damage is severe, your doctor may recommend surgery. Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
Stretching Exercises
Strengthening exercises. Below are two simple strength exercises to help condition the muscles, tendons and joints around the foot and ankle. Plantar Rolling. Place a small tin can or tennis ball under the arch of the affected foot. Slowly move the foot back and forth allowing the tin can or tennis ball to roll around under the arch. This activity will help to stretch, strengthen and massage the affected area. Toe Walking. Stand upright in bare feet and rise up onto the toes and front of the foot. Balance in this position and walk forward in slow, small steps. Maintain an upright, balanced posture, staying as high as possible with each step. Complete three sets of the exercise, with a short break in between sets, for a total of 20 meters.